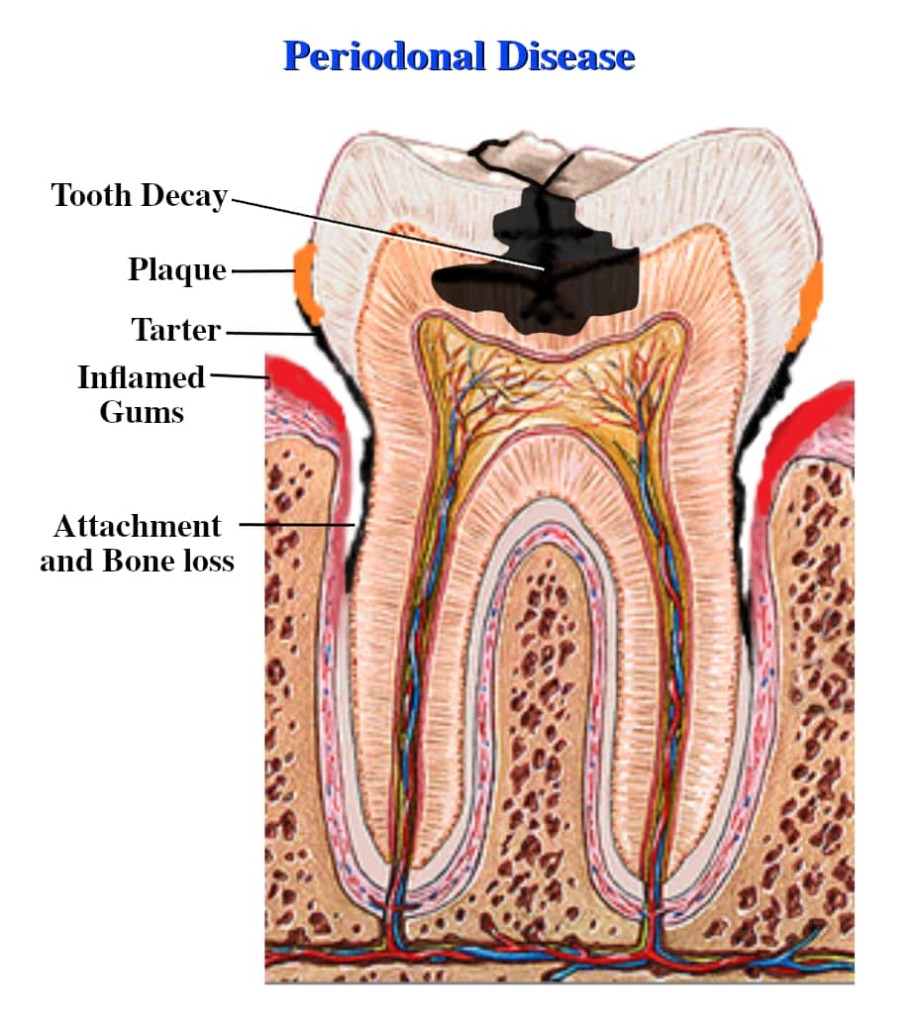
There are many reasons for teeth loss. But they mostly have to do with Periodontal Disease—infection of what’s called your Periodontium, which includes your gums and the anotomical structures underneath them—caused by bacteria that lead to a collection of Plaque and Tarter on the teeth, inflamed gums and Resorption (breakdown and shrinkage) of the gums and other parts of the Periodontium. There are many steps you can take, though, to prevent such disease. We at the Grantham Denture Clinic can help you after you’ve lost one or more of your own natural teeth with different denture options (see below). But why not prevent that teeth loss in the first place? Hopefully this page can help you understand those preventative steps by understanding the Periodontium and Periodontal Disease, or at least help you understand a little bit about the process that led to your teeth loss should that already have happened.
There are many reasons for teeth loss. But they mostly have to do with Periodontal Disease—infection of what’s called your Periodontium, which includes your gums and the anotomical structures underneath them—caused by bacteria that lead to a collection of Plaque and Tarter on the teeth, inflamed gums and Resorption (breakdown and shrinkage) of the gums and other parts of the Periodontium. There are many steps you can take, though, to prevent such disease. We at the Grantham Denture Clinic can help you after you’ve lost one or more of your own natural teeth with different denture options (see below). But why not prevent that teeth loss in the first place? Hopefully this page can help you understand those preventative steps by understanding the Periodontium and Periodontal Disease, or at least help you understand a little bit about the process that led to your teeth loss should that already have happened.
Patient Information
Understanding Teeth Loss
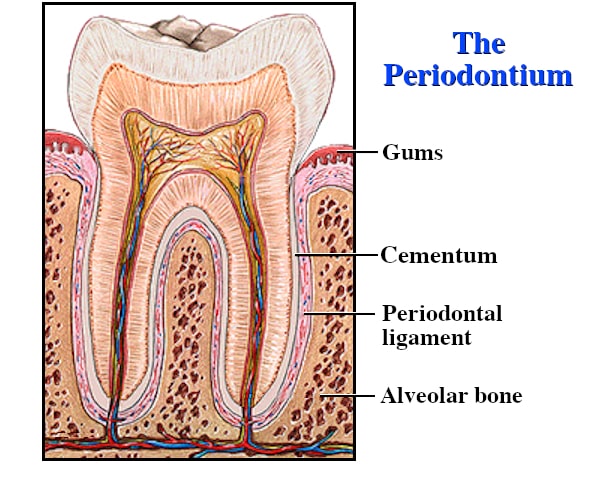
Parts of the Mouth Involved in Chewing: The Periodontium
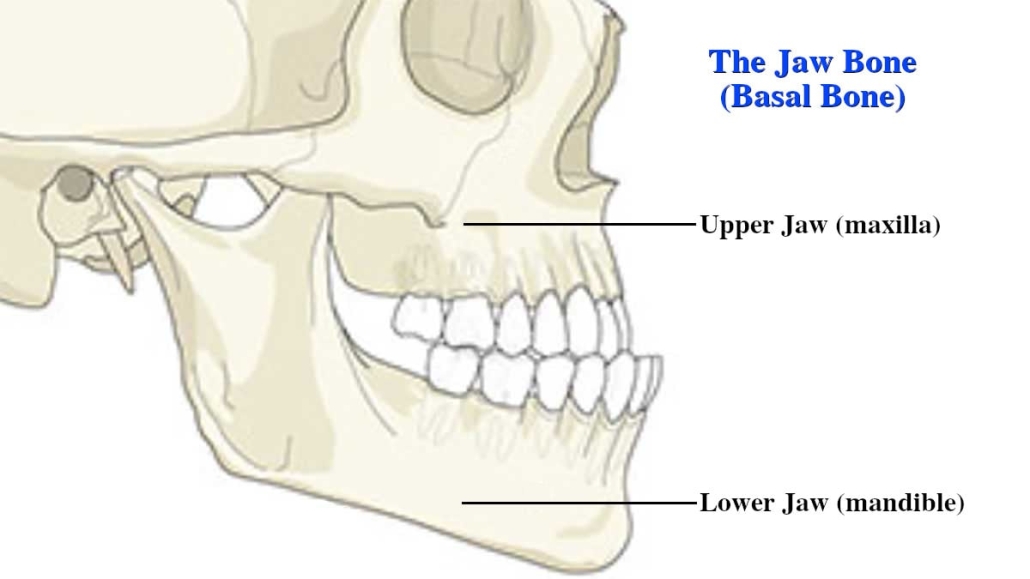
- Jaw Bone (bottom diagram): (i) The lower jaw (mandible) supports the bottom row of teeth and gives shape to the lower face and chin. This is the bone that moves as the mouth opens and closes. (ii) The upper jaw (maxilla) holds the upper teeth, shapes the middle of the face and supports the nose. >>> Note that one way to talk about the jaw bone is to say it is made up of the Basal Bone (a very hard bone) and the Alveolar Bone (a softer bone that sits on top of the basal bone and in which the natural teeth are embedded). Or we can talk about the jaw bone as just being the basal bone in order to distinguish the Alveolar Bone so that we can talk about its role in the Periodontium (top diagram).
- Alveolar Bone (top diagram): On top of the jaw bone is the alveolar bone (a.k.a. alveolar ridge or alveolar process). It’s a thickened ridge of bone that contains—or once contained—the tooth sockets on the jaw bone.
- Periodontal Ligament: On top of the alveolar bone is the periodontal ligament (a.k.a. PDL), a group of specialized connective tissue fibres that essentially attach a tooth to the alveolar bone within which it sits.
- Cementum: A specialized calcified substance covering the roots of the teeth that attaches the teeth to the alveolar bone by anchoring the periodontal ligament.
- Gums: On top of the periodontal ligament are the Gums (a.k.a. gingiva (or the plural: gingivae)). The gums are the soft tissue that surround the natural teeth if there are any or what the denture sits on if not. They function to provide a seal around the natural teeth and a cushion between the natural teeth or denture and the deeper tissues—the underlying ligaments and bone. The gums function to absorb the forces created during the biting down process and chewing of food.
Changes to the Periodontium
We may not realize this, but the jaw bones, like all bones, are living tissue (specifically a specialized connective tissue) which have their own blood vessels and are made of various cells, proteins, minerals and vitamins. This structure enables them to grow, transform and repair themselves throughout life. Bone is normally subjected to a constant regeneration process. It therefore goes without saying that the Periodontium (the alveolar ridge, periodontal ligaments and gums sitting on top of the jaw bones) are similarly living tissue as well, undergoing constant change. It is the repeating stress on the jaw bones and Periodontium caused by the forces exerted by our natural teeth biting down and chewing that continuously stimulates the breaking down (Resorption) and Regeneration process of the bone and tissue cells.
But when we begin to experience Periodontal Disease (infection of our gums and other parts of the Periodontium), we have a problem. Periodontal disease is caused by dental Plaque, which contains harmful bacteria. The mouth is full of bacteria but they tend to be harmless varieties. Periodontal disease usually develops because of an increase in bacteria quantity in the oral cavity and a change in balance from harmless to disease-causing bacteria. These harmful bacteria increase in mass and thickness until they form a sticky residue called Plaque. When plaque growth accumulates to excessive levels, it will cause inflammation and infection of periodontal structures. When plaque is allowed to remain in the periodontal area, it becomes mineralized and transforms into calculus (commonly known as Tartar). This material has a rock-like consistency and grabs onto the tooth surface. Tartar is much more difficult to remove than plaque, which is a soft mass.
Prevention of periodontal disease is obviously the best practice, beginning with good and consistent dental hygiene: brushing gently (not too hard or aggressively) twice daily with a fluoride toothpaste, and cleaning between the teeth with floss or an interdental cleaner. Also eating a well-balanced diet is important to keep the entire Periodontium and the immune system healthy.
Receding Gums
Unfortunately, gum recession cannot be reversed—per se. There is currently no cure for gum recession or disease, but it can be managed if done so with diligence and care. When gum recession takes hold, the gums become inflamed and more red, and the gum line around some teeth “sinks” or looks lower than other teeth, actually exposing the roots. Root surfaces are softer than tooth enamel and so are more prone to erosion and are more sensitive to heat, cold and even sweets. They can get so worn that the teeth loosen or break. Some people also notice their bite is different or uncomfortable, the gums are tender or they have pain in the mouth.
Have you noticed your gums pulling back from your teeth, or do your teeth look longer? If so, you likely have receding gums. Gum Recession happens when the bone and tissues underneath the gums undergoes Resorption (shrinkage) and disappears, making the gums pull back and exposing the root surface of teeth—if you have any left. It can be localized, affecting one or two teeth, or generalized. Receding gums result from a number of different causes, the most serious being Periodontal (gum & underlying bone) Disease, as discussed above.
- Periodontal (gum) disease
- Poor oral hygiene (e.g. brushing, flossing)
- Brushing your teeth too hard and aggressively or too many times a day
- Using a toothbrush with stiff bristles
- Old age
- Poorly fitting dentures
- Smoking or chewing tobacco
- Certain prescription medications
- Diabetes
- Genetics
- Sports injury or similar trauma
- Teeth that are out of alignment
- Grinding your teeth at night
- Other causes of the accumulation of bacteria: e.g. damage from dental treatment, such as fillings and crowns placed too deep into the gums
Even though the tissue will not grow back, there are specific steps to take to keep the recession from getting worse. Better oral care habits such as brushing your teeth gently twice a day for two minutes each, using a toothbrush with softer bristles and such things as plaque-fighting mouth rinse and dental picks can all be discussed with your dentist. Successful treatment ultimately depends on how your gum recession originated in the first place.
Dentures, Receding Gums & Other Periodontium Resorption
Many people, unfortunately, do begin to loose their natural teeth, especially as they age. You can do whatever you can—and you should do whatever you can—to slow down tooth loss, but many factors, such as genetics and your dental history throughout your life, inevitably lead to Receding Gums and other parts of the Periodontium undergoing Resorption, as discussed above. Eventually a time comes where you, together with your denturist and dentist, decide you need dentures.
 * As already mentioned above, one of the benefits of Implants (which are surgically screwed into the Alveolar Bone or both the Alveolar & Basal Bones of the jaw) and Implant Dentures is to slow down the bone and tissue shrinkage by continually stimulating the bones and tissues via the biting down forces. You can read more about this under Advantages of Implant Dentures on our FAQ page.
* As already mentioned above, one of the benefits of Implants (which are surgically screwed into the Alveolar Bone or both the Alveolar & Basal Bones of the jaw) and Implant Dentures is to slow down the bone and tissue shrinkage by continually stimulating the bones and tissues via the biting down forces. You can read more about this under Advantages of Implant Dentures on our FAQ page.
As your Periodontium continues to change, you may need an Adjustment to your denture from time to time if you begin to feel some discomfort. Just call us to book a quick appointment for your denturist to make that adjustment.
Call us to book your Free Consultation appointment
or discuss more with us on the phone!
Call us to book your
Free Consultation appointment
or discuss more with us
on the phone!